The Risks That Come With Crowded Teeth
By Dr. Emily Watson
Cheryl’s problem with crowded teeth began when she was a child.
The problem didn’t end until she was in her 50s and had undergone double jaw surgery, which is a reminder that crowded teeth can sometimes be a cause of distress for both children and adults, not to mention dentists and orthodontists.
But before we dive too much into Cheryl’s specific case, let’s take a moment to explore the problems teeth crowding can cause in general.
To begin with, any number of causes can lead to crowded teeth. Sometimes it’s genetics, with smaller jaws simply being a family trait. In other cases it might be a dental abnormality of some sort, such as an extra tooth or impacted teeth. Thumbsucking or too much pacifier use as a small child can also contribute to a narrower upper jaw and less space for the teeth. So can losing a baby tooth too soon. That creates a space for other teeth to move into, making it more difficult for permanent teeth to claim their rightful spot when the time arrives. With so many causes, there are plenty of opportunities for teeth to wedge themselves in too closely.
And that’s definitely not good. Crowded teeth are difficult to clean because the space between them is abnormally tight, so unless you give extra care when brushing and flossing this can lead to increased risk of cavities. In Cheryl’s case, crowding was a symptom, not a cause. She had crowding as a child, hence teeth were pulled; however, why is she still crowded now as an adult?
By the time Cheryl arrived in my office as a new patient, she had a history of teeth crowding that dated back decades.
When she was a girl, a dentist spotted the problem of too many teeth trying to claim ownership of too little space in her mouth and pulled four of her teeth, creating room for the remaining 28 to flourish.
That worked.
For a while.
The Movement of Teeth
Years passed. One thing many people may not know about teeth is that they don’t remain still, even though it appears that they do. They move, subtly, in such an incremental way that day to day, month to month, and year to year you are unlikely to notice that your teeth are on a journey, although one in which the distance is barely measurable. And as you get older, the direction all of your teeth are moving in is toward the midline of your mouth. The ones on the right side move toward the midline, and the ones on the left side move toward the midline, pushing against each other like a line of concert goers impatient for the arena doors to open.

This is what Cheryl experienced, although as it was happening, she was as unaware as anyone would be.
It was all about to be revealed, though, because when a new patient arrives in our office they are handed a sleep questionnaire. (That may sound irrelevant to the problem of crowded teeth, but there are connections.) The sleep questionnaire is something recommended by the American Dental Association and I am a big proponent of it. Sleep questionnaires ask patients whether they snore, feel drowsy during the day, or experience any of a long list of other sleep-related difficulties. Cheryl answered with a sea of “yeses” all the way down the questionnaire. Just about any type of problem with sleep you could name, she experienced it.
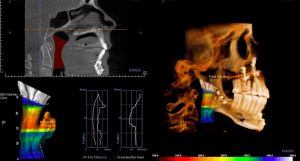
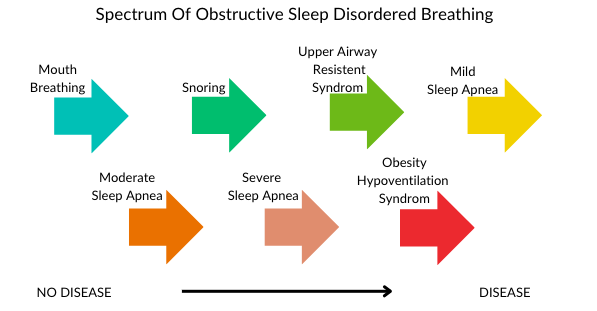
When I sat down to talk with Cheryl, one of the things I addressed was how narrow her palate was and that this was because she breathed through her mouth, not through her nose, which of course is a symptom of dysfunctional oral rest postures and mouth breathing. She had not even realized that her mouth breathing was a problem. She had breathed that way all her life and no one raised any concerns or suggested she might want to work on breathing through her nose. But mouth breathing can be the start on a spectrum of what eventually may progress to disease and show up as sleep apnea.
Meanwhile, sleep apnea brings its own set of health concerns, including raising the risk of high blood pressure, diabetes, heart disease, and stroke.
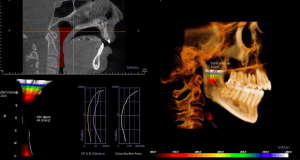
I recommended Cheryl see an oral surgeon for jaw surgery. Of course, no one wants to hear that kind of recommendation, but I kept thinking about how Cheryl thought that what she was experiencing was normal, and how terrible it must have been to have lived like that all these years.
I told her, “If you were my mom, and I knew the effect sleep apnea was having on your quality of life, I would want you around as long as possible. If that means jaw surgery, I would want that for you.”
Addressing Other Difficulties
Of course, ideally you would want to avoid jaw surgery because it would save the patient a lot of discomfort, but in some cases there’s no getting around it.
Cheryl had the double jaw surgery last year and has done well since. But she has also needed to take other measures to conquer her problems with mouth breathing and sleep apnea. She has been participating in myofunctional therapy, which is a sort of physical therapy for the mouth where the therapist retrains the person on proper breathing and swallowing, as well as where to rest the tongue. Proper tongue placement (at the roof of your mouth when it is resting) is critical to good breathing habits.
Cheryl also had a deviated septum. The septum is the wall between your right nostril and left nostril, and sometimes it is off center. When that happens, one nostril can become partially blocked, making breathing more difficult. So I sent Cheryl to an ear, nose, and throat specialist and she had surgery on her nose.
Finally, she was also fitted for braces.
It’s been quite the journey for Cheryl, but now things are looking up and she can breathe easier – literally.